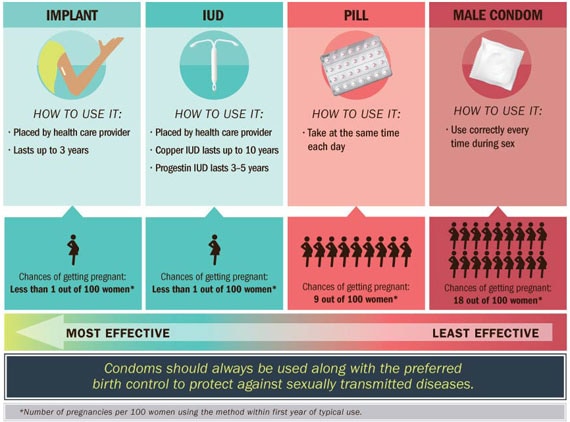
Teen childbearing can carry health, economic, and social costs for mothers and their children. Teen births in the US have declined, but still more than 273,000 infants were born to teens ages 15 to 19 in 2013. The good news is that more teens are waiting to have sex, and for sexually active teens, nearly 90% used birth control the last time they had sex. However, teens most often use condoms and birth control pills, which are less effective at preventing pregnancy when not used consistently and correctly. Intrauterine devices (IUDs) and implants, known as Long-Acting Reversible Contraception (LARC), are the most effective types of birth control for teens. LARC is safe to use, does not require taking a pill each day or doing something each time before having sex, and can prevent pregnancy for 3 to 10 years, depending on the method. Less than 1% of LARC users would become pregnant during the first year of use.
Doctors, nurses, and other health care providers can:
- Encourage teens not to have sex.
- Recognize LARC as a safe and effective choice of birth control for teens.
- Offer a broad range of birth control options to teens, including LARC, and discuss the pros and cons of each.
- Seek training in LARC insertion and removal, have supplies of LARC available, and explore funding options to cover costs.
- Remind teens that LARC by itself does not protect against sexually transmitted diseases and that condoms should also be used every time they have sex.
Problem: Few teens (ages 15 to 19) on birth control use the most effective types.
Use of Long-Acting Reversible Contraception (LARC) is low.
- Less than 5% of teens on birth control use LARC.
- Most teens use birth control pills and condoms, methods which are less effective at preventing pregnancy when not used properly.
- There are several barriers for teens who might consider LARC:
- Many teens know very little about LARC.
- Some teens mistakenly think they cannot use LARC because of their age.
- Clinics also report barriers:
- High upfront costs for supplies.
- Providers may lack awareness about the safety and effectiveness of LARC for teens.
- Providers may lack training on insertion and removal.
Providers can take steps to increase awareness and availability of LARC.
- Title X is a federal grant program supporting confidential family planning and related preventive services with priority for low-income clients and teens.*
- Title X-funded centers have used the latest clinical guidelines on LARC, trained providers on LARC insertion and removal, and secured low- or no-cost options for birth control.
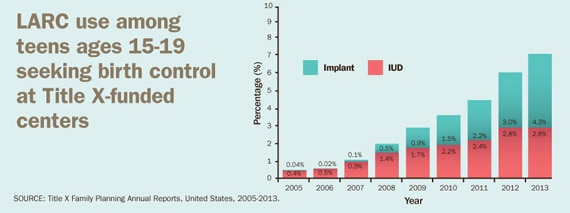
- Teen use of LARC has increased from less than 1% in 2005 to 7% in 2013.
- Other state and local programs have made similar efforts.
- More teens and young women chose LARC, resulting in fewer unplanned pregnancies.
LARC use among teens ages 15-19 seeking birth control at Title X-funded centers
SOURCE: Title X Family Planning Annual Reports, United States, 2005-2013.
How effective is LARC at preventing pregnancy compared with other birth control commonly used by teens?